Abstract

Introduction. Immune Thrombocytopenia (ITP) is usually a benign and self limiting condition in children, although sometimes bleeding can be severe and treatment may be required. New international recommendations and ASH guidelines were published in 2011 however a recent North American review demonstrated that most most children continue to receive therapy. In contrast previous UK analysis in 2011 has demostrated successful avoidance of therapy for most children.
Objective. The aim of this study was to assess the proportion of children in UK with newly diagnosed ITP, their bleeding sseverity and the treatment given. These outcome were compared to previous UK findings. A more ddetailed analysis was undertaken on children with moderate bleeding whom are the population were the need for intervention can be most unclear.
Methods. Data was extracted from the UK ITP Childhood registry of all patients diagnosed with ITP from January 2010 to May 2017. Bleeding severity was assessed according to the Bolton-Maggs and Moon severity scale.
Results. Data from 1003 patients was analysed. 46.2% of the children had mild bleeding, 49.7% had moderate bleeding and 4.1% had severe or life-threatening bleeding, with bruising and petechiae being the most common manifestations. 37 childrenhad severe or life threatening bleeding; 15 had epistaxis, 8 had menorrhagia, 5 had oral haemorrhage, 8 had Gastrointestinal bleeding, 3 had ICH and 2 had macroscopic haematuria.
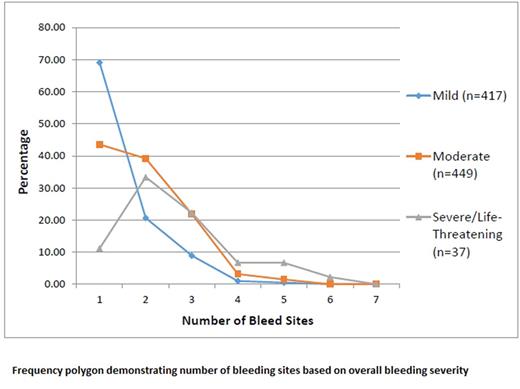
Children with mild bleeding had a lower mean number of bleeding sites (1.4) compared to the children with moderate (1.9) and severe (2.6) bleeding. The proportion of children receiving treatment was 8.4% for mild, 22.3% for moderate and 64.9% for severe bleeding. The most common treatment was steroids (42.3%), followed by IVIG (40.5%) or a combination of both (15.3%).
These figures have not changed significantly since the database was reviewed between 2007-2009. Children with moderate bleeding who were treated had a median of 3 bleeding sites compared to 2 in those who were not treated.
Conclusion. There has been no change in the trend of management of ITP in the UK since previous analysis or following new guidelines. This review suggests that the number of bleeding sites is the best predictor for need of platelet rising therapy.
Grainger: Novartis: Honoraria; GSK: Honoraria; Amgen Inc.: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal